When Should Women Start Regular Cervical Screening?
Maintaining reproductive health is an important part of overall wellbeing for women across Australia. One area that often raises questions is the timing of routine checks for the cervix. National guidelines have changed over time based on medical research, leading to clearer recommendations about; when testing should begin and how often it should be done.
This article explains the current Australian approach, why age-based recommendations exist, and how regular participation supports early identification of potential concerns. The information is intended to help readers make informed choices and understand what to expect, rather than replace advice from a qualified health professional.
Understanding Cervical Health and Why Screening Matters
The cervix is the lower part of the uterus that connects to the vagina. Changes in cervical cells often develop slowly and may not cause symptoms in the early stages. Without routine testing, these changes can go unnoticed for years.
Regular testing allows healthcare providers to identify abnormal cell changes before they progress. As part of broader preventive healthcare services, this approach has significantly reduced the rate of cervical cancer in Australia, particularly since the introduction of organised national screening programs. Early detection not only improves treatment outcomes but may also reduce the need for more invasive procedures later in life.
When Should Women Start Cervical Screening?
Under current Australian guidelines, women and people with a cervix are advised to begin cervical screening at 25 years of age, regardless of sexual history. This recommendation is based on strong evidence showing that screening before this age does not significantly reduce cancer risk but can lead to unnecessary follow-up procedures.
From age 25 to 74, routine testing is generally recommended every five years if results are normal. This interval reflects improvements in testing accuracy and a better understanding of how cervical cell changes develop over time.
It is important to note that starting age and frequency may differ for individuals with specific medical histories, weakened immune systems, or previous abnormal results.
Why Screening Does Not Start Earlier
Earlier guidelines once encouraged testing from a younger age, but research has shown that the human body often clears HPV infections naturally in younger women. Testing too early may detect temporary changes that would resolve without treatment.
By starting later, the current approach balances early detection with avoiding unnecessary anxiety and medical intervention. This change has been widely supported by public health experts across Australia.
Understanding the Current Testing Method
Modern screening focuses on detecting human papillomavirus, commonly known as HPV. Certain strains of this virus are linked to changes in cervical cells over time. Identifying the presence of HPV allows healthcare providers to assess risk more accurately than older testing methods.
If HPV is detected, further analysis may be done to check whether any abnormal cell changes are present. When HPV is not found, the likelihood of developing serious cervical conditions within the next five years is considered very low.
How Often Should Women Be Tested?
For most eligible individuals, testing every five years is sufficient. This interval is based on strong evidence showing that HPV-related changes develop slowly.
More frequent testing is not usually required unless recommended by a healthcare professional due to specific medical history, weakened immune system, or previous abnormal results. Following the recommended schedule helps ensure early identification while reducing unnecessary procedures.
Who Should Participate in Regular Checks?
Routine testing is recommended for:
- Women aged 25 to 74
- People with a cervix, including those who have received the HPV vaccine
- Individuals who have been sexually active in the past
Vaccination significantly lowers risk but does not remove the need for ongoing monitoring, as it does not protect against all HPV types.
Special Circumstances That May Affect Timing
Certain life stages or medical histories, such as pregnancy, menopause, or previous cervical procedures, may influence when screening is recommended. In these situations, timing should be guided by individual health needs and professional medical advice rather than standard schedules.
Pregnancy
If a test is due during pregnancy, it can usually be performed safely. Timing should be discussed with a healthcare provider to ensure comfort and suitability.
After Menopause
Even after periods have stopped, regular checks remain important until the upper age limit, as cellular changes can still occur.
Following a Hysterectomy
People who have had a total hysterectomy may not require further testing, depending on the reason for surgery and previous results. Individual medical advice is essential.
Recognising Symptoms Between Scheduled Tests
Routine checks are designed to identify changes before symptoms appear. However, medical advice should be sought if any of the following occur:
- Bleeding outside of normal menstrual cycles
- Bleeding after intercourse
- Persistent pelvic discomfort
- Unusual vaginal discharge
These symptoms can have many causes and do not always indicate serious illness, but timely assessment is important. Appointments with a general practitioner can be arranged through trusted booking platforms that support public healthcare access, including the ability to book a GP appointment online.
Addressing Common Misunderstandings
Clear, evidence-based information helps dispel common myths about cervical screening and supports informed health decisions.
“I feel healthy, so testing is unnecessary”
Many cervical changes cause no symptoms in the early stages. Feeling well does not always reflect underlying cellular changes.
“I am no longer sexually active”
HPV exposure can occur many years before changes develop, which is why past sexual activity remains relevant.
“The procedure is painful”
Most people experience mild discomfort rather than pain. Healthcare providers aim to make the process as comfortable as possible.
The Role of General Practice in Women’s Health
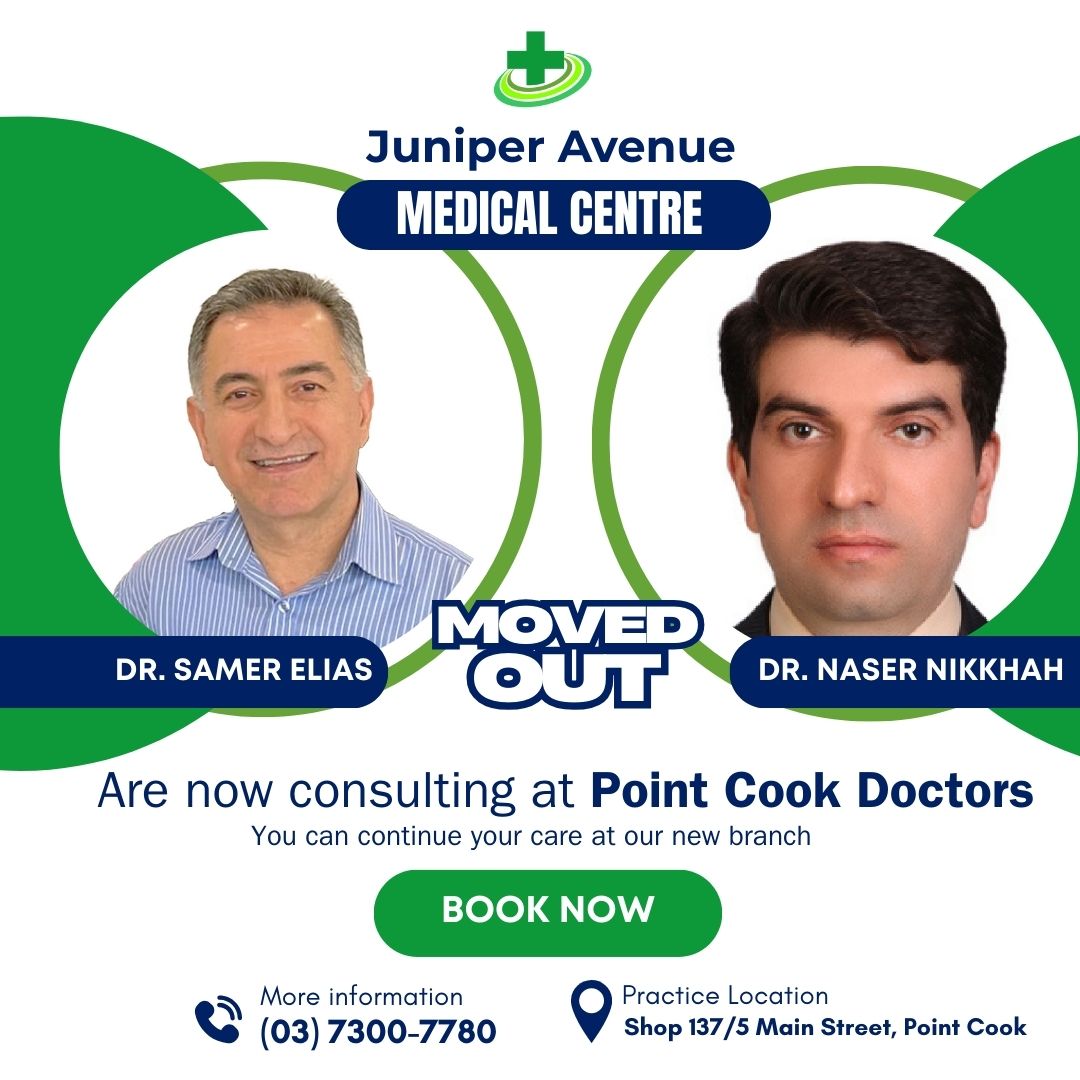
GP guide patients on appropriate testing schedules, explain results, and arrange follow-up care when needed, while considering cervical health as part of overall wellbeing. Accessing care through a general practice clinic in Point Cook allows patients to receive evidence-based advice aligned with Australian guidelines, with Juniper Avenue Medical Centre supporting community access to preventive healthcare.
Importance of Staying Informed
Public health recommendations evolve as medical knowledge advances. Staying informed about current guidelines helps women make confident decisions and reduces uncertainty around testing schedules.
Understanding why testing begins at a specific age and why intervals are set several years apart can ease concerns and encourage consistent participation.
When to Seek Further Advice
Questions about personal risk, medical history, or previous test results should always be discussed with a qualified healthcare professional. Individual circumstances can influence recommendations. For further information or to speak with a healthcare provider, patients can contact the medical centre to access appropriate guidance and support.
Key Takeaways
- Routine checks begin at age 25 under Australian guidelines
- Testing every five years is sufficient for most individuals
- Vaccination does not replace the need for ongoing monitoring
- Early detection supports better long-term outcomes
Cervical screening remains a cornerstone of women’s preventive healthcare in Australia. By understanding when to begin and why it matters, women can take an active role in protecting their long-term health with confidence and clarity.
Final Thoughts on Cervical Health Awareness
Knowing when to start regular checks and why they matter empowers women to take an active role in their long-term health. Australia’s screening guidelines are based on extensive research and are designed to offer the greatest benefit with minimal harm. By staying informed, attending scheduled tests, and seeking medical advice when something does not feel right, women can significantly reduce their risk of developing serious cervical conditions. Juniper Avenue Medical Centre encourages informed decision-making and supports patients through accessible, preventive healthcare services across Australia. Parents can book an appointment online to discuss immunisations or other preventive care for their children.